By Consultant Diabetologist Dr. V. Nallaperumal
Juvenile diabetes is usually diagnosed in children and young adults, and is classified as Type 1 diabetes. In type 1 diabetes, the pancreatic beta cells do not produce insulin. Insulin is necessary for the body to be able to use glucose.
Glucose is the basic fuel for the cells in the body, and insulin takes the glucose from the blood into the cells. Since Type 1 patients lack insulin secretion altogether, they need an external supply of insulin to live. Since they are dependent on insulin for survival, their disorder was previously classified as Insulin Dependent Diabetes Mellitus (IDDM).
For the child, this diagnosis implies a lifetime on insulin injections with frequent pricks for blood glucose testing, restrictions in diet and physical activity, regular visits to the doctor and living in constant fear of hypoglycemia and diabetic coma. If not efficiently managed, the child with Type 1 diabetes will be deprived of the normal pleasures and carefree existence that one associates with this phase of life.
Common causes of Type 1 Juvenile Diabetes:
- Autoimmune Disease
This is the most common cause of type 1 diabetes. The immune system wrongly perceives the insulin-producing beta cells of the pancreas as a threat and eradicates them. - Hereditary
Diabetes does run in families. A genetic predisposition exists for Type 1 Diabetes. The disease is more common in first-degree relatives compared to the general population. Secondly, it is much more common among identical twins as compared to non-identical twins. - Idiopathic Type 1 Diabetes
In some rare cases, diabetes develops without any apparent cause. This form of diabetes is known as idiopathic type 1 diabetes.
Also read: What is Precision Diabetes? Find out!
Environmental factors of importance include viruses (Coxsackie virus), dietary agents (Cow’s milk protein, nitrosamines found in smoked meat)) and exposure to toxins (Rat poison Vacor, Streptozotocin, Alloxan, Pentamidine).
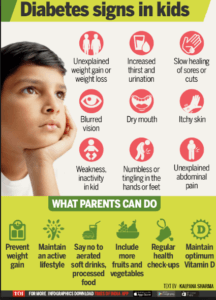
Some of the symptoms of uncontrolled diabetes are excessive thirst and dehydration, frequent urination, hunger, weight loss, blurred vision, weakness, tiredness or sleepiness, vomiting or nausea and sudden irritability.
The clinical onset of diabetes in a child is often rapid with symptoms being present for only a few days or weeks preceding diagnosis. A recent onset of bedwetting in a previously toilet-trained child and vaginal candidiasis (a fungal infection) in prepubertal girls are other important clues to the diagnosis.
Undiagnosed type 1 children can present with acute complications at the time of diagnosis itself. When the body doesn’t have access to glucose for energy because of lack of insulin, it begins to break down fats. Ketones are chemical compounds that result from the breakdown of fat. They are toxic, and can kill cells. Left unchecked, high levels of ketones can cause a diabetic coma.
Pic courtesy: TimesOfIndia
Treatment of Juvenile Diabetes:
- To maintain normal growth and development
- To keep blood sugar levels within a target range (not too high, not too low) as much as possible
- To promote emotional well-being
Blood sugar testing must be performed several times throughout the day, and is an essential part of diabetes management. Every three or four months a glycosylated haemoglobin test (HbA1c) may also be performed. The test indicates how effectively the patient has been managing his or her blood sugar levels over the last two to three months.
People diagnosed with type 1 diabetes usually start with two injections of insulin per day of two different types of insulin and generally progress to three or four injections per day of insulin of different types. The types of insulin used depend on their blood glucose levels. Studies have shown that three or four injections of insulin a day give the best blood glucose control and can prevent or delay the eye, kidney, and nerve damage caused by diabetes.
Raising a child, with or without diabetes, is never easy. Diabetes doesn’t change the basics of parenting. However, it adds new challenges, from birth to the teenage years.
Treatment of diabetes in children under the age of seven falls largely to the parents. Young children cannot be expected to be responsible for their own blood tests, or to follow a diabetic diet without supervision.
The child should be actively involved in diabetes management whenever possible. After all, childhood diabetes does not go away with age. Young children should be made aware that diabetes is not a punishment, and is certainly not their fault.
Eating meals at about the same time every day helps keep blood sugar levels in the target range. Children with diabetes often need to eat snacks during the day and before, during, or after exercise. Children with diabetes can – in fact, they should – play games and sports with their friends. Exercise helps to lower blood sugar levels. Because children’s lives involve a lot of unplanned activity, it’s a good idea for the child to always carry snack foods.
Also read: On choosing the right footwear for diabetics
School-age children School-age children want to be like their peers. It’s not unusual for children with diabetes to feel “different” because they need insulin shots, check blood sugar regularly, and use a meal plan.
It’s not uncommon for a child to believe that their diabetes is actually some form of punishment. Children have to deal with what they perceive as unfair restrictions (“How come he gets to eat all that ice cream and I don’t?”), overprotective family members, guilt and resentment.
Staff at the child’s school need to know about the child’s diabetes. At the beginning of the school year, such a child’s parents should arrange a meeting with the child’s teachers, coaches, the principal, and other school staff. They should be provided with information such as:
- when to check blood sugar and take insulin
- meal and snack times
- preferred snacks and party foods
- usual symptoms of high or low blood sugar
- preferred treatment for high or low blood sugar
- phone numbers for emergencies
Teenagers For the teenager with diabetes, having to take insulin, check blood sugar, and use a meal plan is bothersome. Diabetes often adds to the normal difficulties of growing up. It is not unusual for a teen with diabetes to ease up on diabetes care and try to act “like everyone else.
Teens often rebel against the restrictions of a diabetic diet and daily testing. Giving older children as much control over their diabetes treatment as possible may help foster a sense of independence. Parents should try to remember not to be too protective at this stage (easier said than done!).
Pic courtesy: ucsf.edu
