By Consultant Diabetologist Dr.V.Mohan and R. Pradeepa….
Despite the significant medical and technological advances made in managing diabetes, hypoglycemic episodes- the acute complication of diabetes is observed frequently. Hypoglycemia occurs when the plasma glucose levels may be less than 50–60 mg/dl.
An alternative definition is a decrease in the blood glucose level or its tissue utilization that results in demonstrable signs or symptoms. The glucose level at which an individual becomes symptomatic is highly variable.
The aim of management in diabetes is to reduce high blood sugar levels with either insulin or oral drugs, depending on the type of diabetes they have or the severity of their condition. Hypoglycemia occurs most often in people who use insulin to lower their blood sugar than in those individuals who take oral hypoglycemic agents.
Hypoglycemia causes recurrent morbidity in most people with Type 1 diabetes and many with Type 2 diabetes, and it is sometimes fatal. Hypoglycemic episodes in patients with diabetes often go unrecognized, and over time, patients may lose the ability to sense hypoglycemia, increasing their risk. It is often the limiting factor in attempts to achieve euglycemia /normal blood glucose level.
Causes of Hypoglycemia:
Causes of hypoglycemia are varied. Mild hypoglycemia occurs in more than half of all diabetic patients who are undergoing treatment. Individuals who have a family history of Type-2 diabetes or insulin-resistance syndrome (ie, hypertension, hyperlipidemia, obesity) may be at higher risk for developing hypoglycemia. The various causes are:
- Medication changes or overdoses
- Infection
- Missing or delaying a meal
- Consuming too little food for the amount of insulin taken
- Excess alcohol consumption
- Metabolic changes over time
- Activity changes
- Any combination of the above factors
Symptoms of Hypoglycemia :
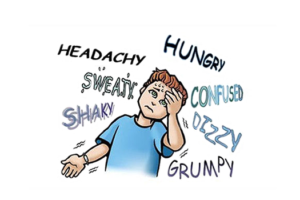
As hypoglycemia occurs as a result of excessively low blood glucose levels, the level of glucose that produces symptoms of hypoglycemia varies from person to person and for the same person under different circumstances.
Hypoglycemia usually occurs gradually and is generally associated with typical warning signs. Hypoglycemic symptoms are related to the brain and the sympathetic nervous system. Symptoms include behavioral changes, hallucinations, focal impairments (eg, hemiplegia), cognitive dysfunction, seizures and eventually, coma and death.
What happens during Hypoglycemia:
Focal neurological deficits occur occasionally. A hypoglycemic episode is not ordinarily associated with a loss of consciousness or a seizure. However, if warning signs are absent or ignored and the blood glucose level continues to fall, more severe hypoglycemia may lead to an alteration of mental function that proceeds to confusion, stupor, and finally to unconsciousness.
Most individuals with diabetes never suffer such severe hypoglycemia. Stimulation of the sympathetic nervous system (Neurogenic symptoms) leads to sweating, palpitations, tremor, anxiety, paresthesias and hunger. Symptoms of hypoglycemia are characteristic and are unique to a given individual. Thus, many people with diabetes learn their symptoms based on their experience.
Hypoglycemia in Type 1 diabetes :
Hypoglycemia occurs most often in people with Type 1 diabetes. Those striving to improve or maintain glycemic control suffer countless numbers of episodes of asymptomatic hypoglycemia. They suffer an average of two episodes of symptomatic hypoglycemia per week and thousands of such episodes over a lifetime of diabetes. An estimated 2–4% of deaths of people with Type 1 diabetes have been attributed to hypoglycemia.
Hypoglycemia in Type 2 diabetes :
Early in the course of Type 2 diabetes, patients may experience episodes of hypoglycemia several hours after meals. The symptoms generally are brief and respond spontaneously. While it is difficult to assess the absolute rates, the frequency of hypoglycemia is substantially lower in Type 2 than in Type 1 diabetes. The rates of severe hypoglycemia in Type 2 diabetes are roughly 10% of those in Type 1 diabetes even during aggressive therapy with insulin.
They are undoubtedly even lower in those treated with oral hypoglycemic agents. Although the episodes are much less frequent overall, the physical and psychosocial morbidity of hypoglycemia in Type 2 diabetes is plausibly assumed to be similar to that in Type 1 diabetes. Mild hypoglycemia is common in patients with Type 2 diabetes undergoing aggressive diabetes management, but severe hypoglycemia is rare. Concerns about hypoglycemia should not prevent efforts to achieve tight glycemic control in most patients with Type 2 diabetes.
Complications of hypoglycemia :
As glucose is the obligate fuel to the brain, during hypoglycemic episode when the glucose concentration of the blood is insufficient to meet the metabolic requirements of the brain, its function deteriorates resulting in cognitive dysfunction.
Cognitive dysfunction during hypoglycemia appears to be more profound in diabetic than in non-diabetic subjects, suggesting that individuals with diabetes have an increased susceptibility to the condition termed neuroglycopenia, which is decreased levels of glucose leading to deficient cerebral glucose availability. This results in confusion, difficulty with concentration, irritability. Injuries are also observed in hypoglycemic-induced brain damage.
Impaired cognition by compromising the microvessels of the brain and causing small strokes. These strokes could be small enough that the classic signs of stroke are not apparent but large enough to produce ischemic damage that affects cognitive function. In Type 1 diabetes hypoglycemic coma is a severe complication altering the quality of life because it markedly increases the anxiety of both the patient and his/her family.
It is considered as a major limiting factor in the glycemic management of Type 1 diabetic patients. Being the consequence of numerous causal factors, hypoglycemic coma is not always easy to prevent and may occur as a paroxysmal phenomenon, sometimes without obvious contributing circumstances.

Treatment:
Attempts to avoid hypoglycemia safely are worthwhile because shifting glucose levels towards the non-diabetic range reduces the long-term complications of diabetes. The safest range is to keep blood sugar level between 70 and 130 mg/dl. Patient education and empowerment, appropriate self-monitoring of blood glucose, flexible drug regimens, individualized and prudent glycemic goals, and ongoing professional support are essential.
Careful consideration should be given to all diabetic patients presenting with hypoglycemia. New medications, activity changes, and infection should be considered. Episodes of hypoglycemia can be effectively self-treated by ingestion of glucose tablets or carbohydrate in the form of juice, a soft drink, milk, chocolates, or a meal.
An initial glucose dose of 20 g is reasonable and should be repeated in 15 to 20 minutes if symptoms have not improved or the monitored blood glucose remains low. As the glycemic response to oral glucose is temporary( typically <2 hours), intake of a snack or meal shortly after the plasma glucose concentration is raised is generally advisable.
In some cases, parenteral therapy may be mandatory when a hypoglycemic patient is unable or unwilling (because of neuroglycopenia) to take carbohydrate orally. Parenteral glucagon is can be used to treat hypoglycemia in Type 1 diabetes. Emergency medical help may be needed if the diabetic individual does not recover in a few minutes after treatment for hypoglycemia. Individuals suffering form a severe insulin reaction may require admission to a hospital to stabilize their blood sugar.
Prevention:
Obviously, prevention of hypoglycemia is preferable to its management. It is possible to improve glycemic control while minimizing the risk of hypoglycemia. Reducing the risk of hypoglycemia, while attempting to maintain plasma glucose concentrations as close to the non-diabetic range can be accomplished safely by following the strategies provided below.
Prevention Strategies for Hypoglycemia:
- Regularity of diet, insulin and exercise
- Snacks between meals and bedtime
- Regular blood testing
- Carrying sugar, candy etc.,
- Availability of glucagon at home
- Education regarding subtle signs
- Identification card
